Table of Contents
What is ACL?

The anterior cruciate ligament (ACL) is a strong band inside your knee that controls stability when you twist, jump, or pivot. It connects your thigh bone to your shinbone, acting like a built-in seatbelt for your knee especially during sports and sudden movements.
How do ACL tears?
Most people injure their ACL through:
- Sudden stops or changes in direction (like football, basketball, skiing)
- Awkward landings from jumps
- Twisting accidents during sports or everyday life
Symptoms & Diagnosis
The immediate symptoms usually include pain and swelling after the injury, along with difficulty bearing weight and a restricted range of knee movement. You may need crutches initially to help you mobilise. After a few days, the pain and swelling often reduce, but the feeling of instability typically persists.
It’s important that an ACL injury is diagnosed promptly. A clinical examination is often needed to suspect the injury, and radiological investigations such as an X-ray and an MRI scan are required to confirm the tear and assess for additional damage to nearby structures, including the meniscus or cartilage.
Treatment Options
Treatment depends on the severity of the tear and your activity level.
Non-Surgical (Conservative) Management
Partial tears or mild sprains can often be managed without surgery. This includes:
- The POLICE method – Protection, Optimal Loading, Ice, Compression, Elevation
- Targeted physiotherapy to restore motion and strengthen surrounding muscles
- Temporary bracing for support and stability
This approach suits patients with lower activity demands or minimal instability.
Surgical Treatment (ACL Repair / Reconstruction)
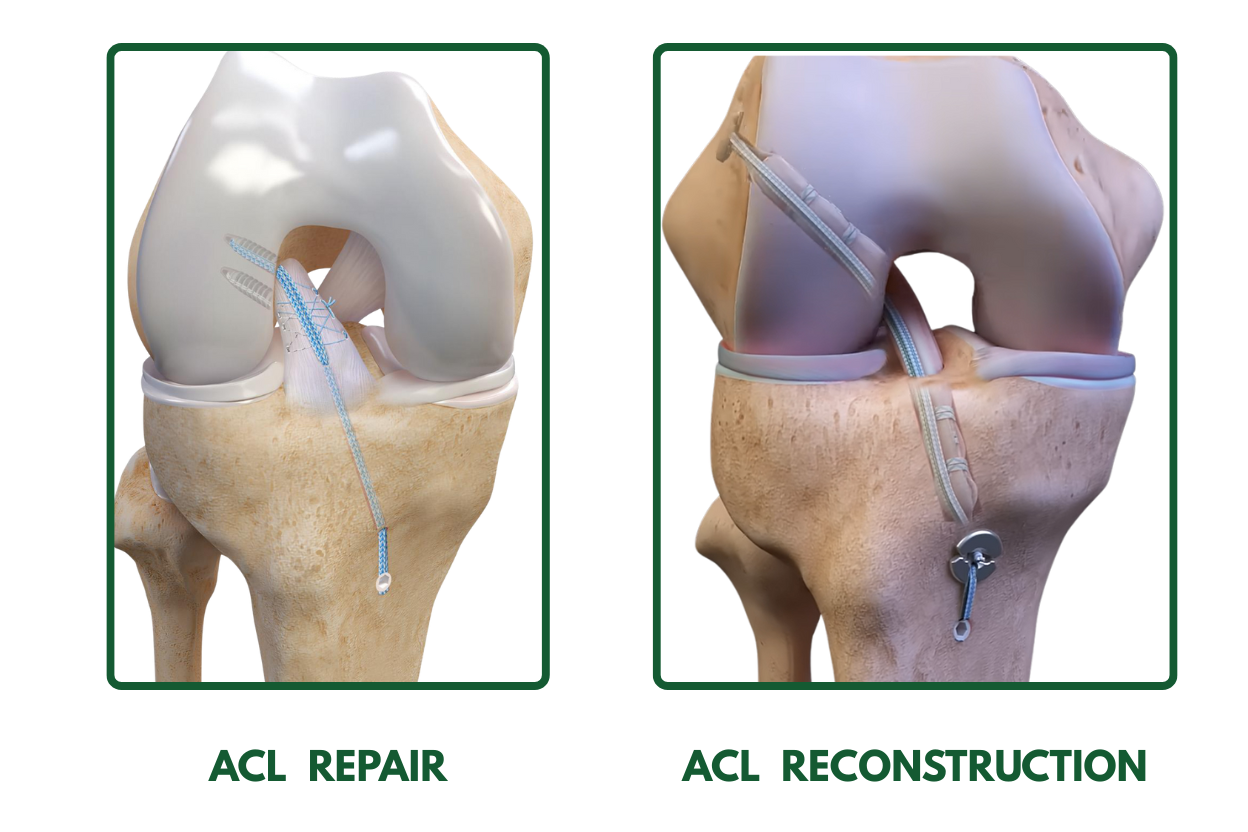
ACL Reconstruction:
Mr. Ellapparadja will perform arthroscopic surgery (keyhole surgery) to reconstruct your ACL.
Advantages of arthroscopic ACL surgery include:
- Small incisions – Less painful and better recovery
- Reduced chances of complications than open surgery.
- Day-case procedure meaning you can go home the same day of surgery.
How ACL Reconstruction is Performed
During ACL surgery, small incisions (keyholes) are made around the kneecap to allow access to the knee joint. An arthroscope with a camera is inserted through one of these incisions, transmitting images to a monitor in the operating room. Through the other keyhole incisions, small surgical instruments are introduced. Your surgeon will then drill small tunnels in the upper and lower leg bones, through which the tissue graft will be anchored.
In most cases, your own tissue, typically a hamstring graft or bone-patellar tendon graft is harvested to reconstruct the ACL. The graft is then secured in place using buttons or screws.
ACL surgery is usually performed under general anaesthesia. Any associated injuries, such as meniscal or cartilage damage sustained during the initial injury, are often treated during the same procedure.
It is essential to attend all your follow-up appointments so your doctor can monitor your recovery and make any adjustments as needed.
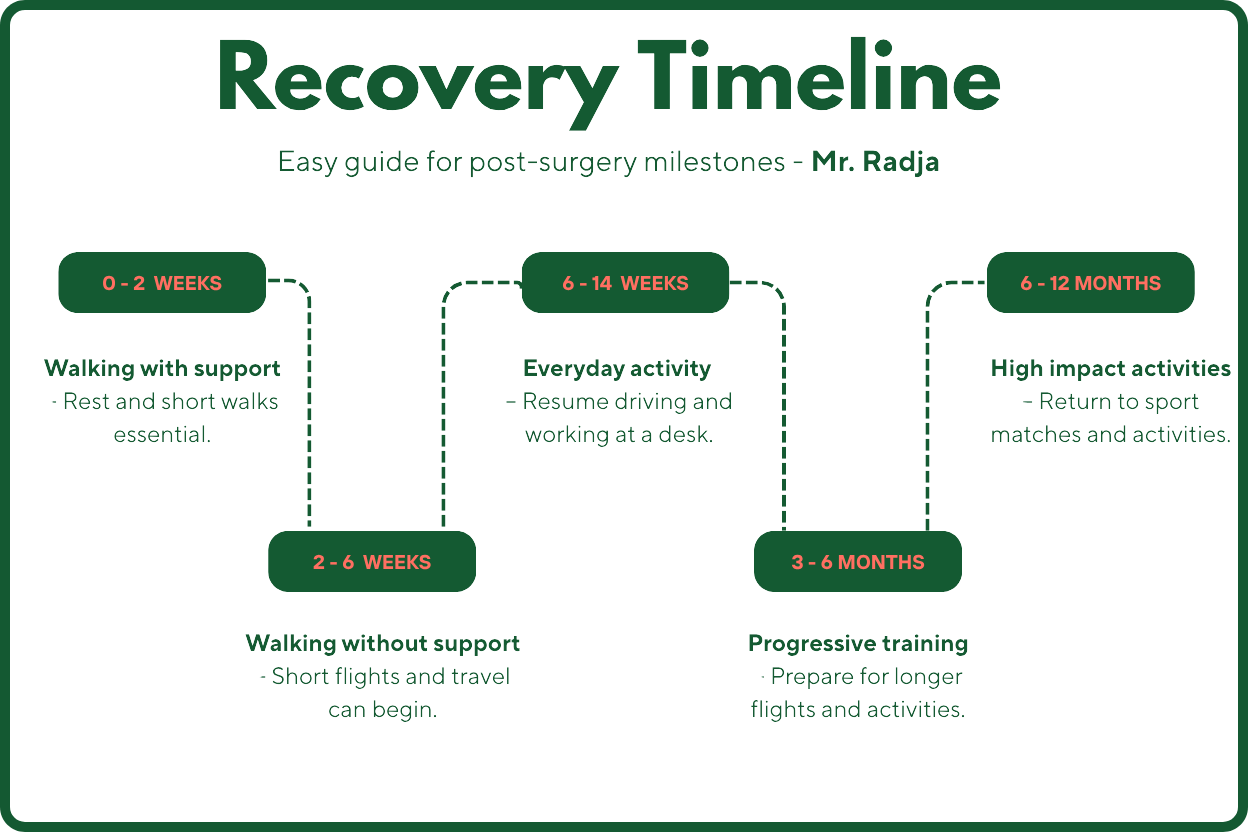
Recovery timeline
After ACL surgery
Since you will be able to go home on the day of the surgery, it is important to have someone drive you, as you may still be recovering from the anaesthesia. Most patients are able to resume driving around 6 weeks after the procedure.
Physiotherapy is an essential part of your recovery. Strength and stability in the knee gradually improve over 4–6 months. Most patients achieve a full recovery when they follow and adhere to physiotherapy guidance. Full recovery can take up to 9 months, although competitive athletes may require a slightly longer period typically 9 months – 1 year to return to high-level sports.
Flying is usually safe after 6 weeks. Remember to stay well hydrated and wear compression stockings during travel.
Risks and complications
Although ACL surgery is generally safe, there are some risks associated with the procedure, including:
- Infection: The risk is low. Your doctor may give you antibiotics before surgery to help prevent infection.
- Blood clots: Patients at higher risk may be prescribed medication to reduce the chance of clots forming. If you have had deep vein thrombosis (DVT) or a pulmonary embolism (PE) in the past, it is important to inform us.
- Weakness or stiffness in the knee: Engaging in physiotherapy, strengthening exercises and regular mobilisation are crucial to preventing these issues.
Re-rupture of the graft: This occurs in about 3–5% of patients. Mr. Radja will assess your knee and discuss further management if this happens.
Lateral Extra-Articular Tenodesis (LET)
Lateral extra-articular tenodesis (LET) is an emerging procedure shown to reduce the risk of graft failure, particularly in high-risk patients. When appropriate, based on patient needs, Mr. Radja may add this procedure to the ACL reconstruction to further minimise the chance of graft failure.
High-Risk Groups Include:
- Young patients (< 28 years)
- Sports personnel (e.g., footballers, skiers, hockey players—sports involving pivoting or cutting movements)
- Individuals with hypermobility or lax joints
- Patients undergoing revision ACL surgery
- Those with a high-grade pivot shift
- Chronic ACL injuries or associated medial meniscal injuries
Summary
An ACL injury can significantly affect your confidence, balance, and ability to stay active but with the right treatment, full recovery is absolutely possible.
If you’re in Manchester and experiencing knee instability, locking, or a “giving way” sensation, it’s important to get assessed early with the expertise of Consultant Knee
Surgeon Mr. Radja.
Understanding your ACL injury is the first step towards both prevention and long-term joint health.
Take care of your knees today to lead active life later years
FAQ
Testimonials
Read all reviews at Doctify.
