Table of Contents
What is Hip Arthritis?
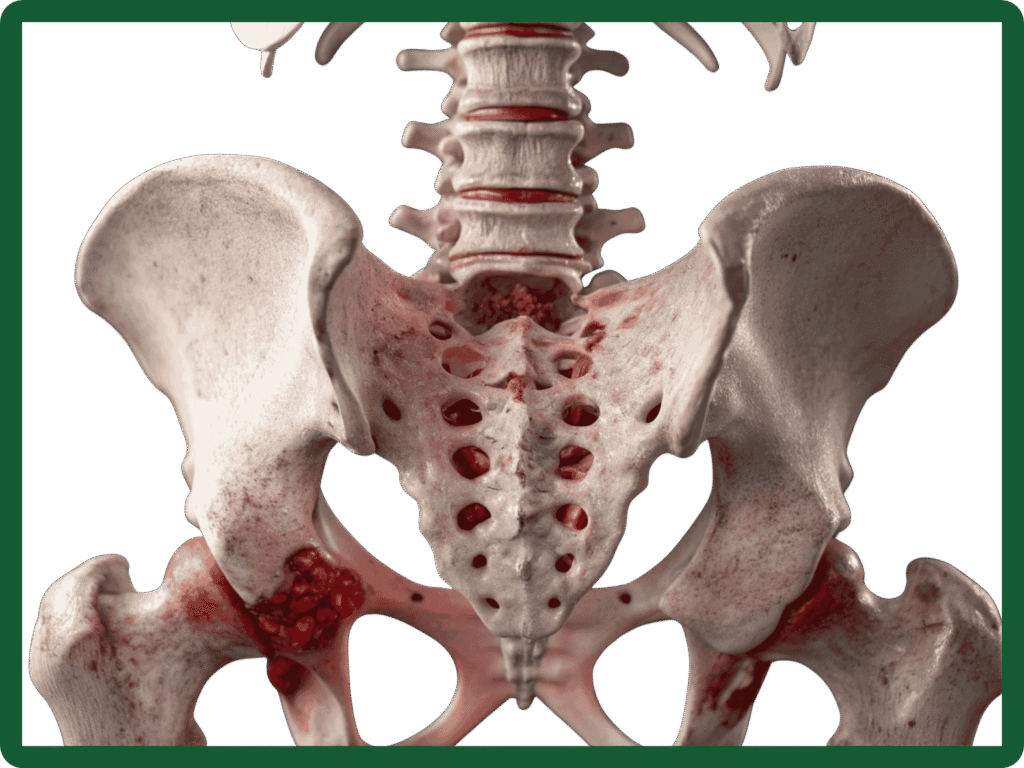
Hip arthritis is the wear-and-tear or inflammation of the hip joint that leads to pain, stiffness and reduced mobility. The hip is a ball-and-socket joint formed by the head of the femur (thigh bone) and the acetabulum (socket) of the pelvis. When the cartilage that cushions the joint wears away, bones rub together, causing pain and limiting everyday activities.
Quick facts
- Most common in people over 50, but can affect younger adults after injury or disease.
- Gradual onset is typical, though symptoms can sometimes follow a fracture or previous hip surgery.
Types of Hip Arthritis
- Osteoarthritis (degenerative): The most common type where cartilage breaks down with age or overuse.
- Rheumatoid arthritis: An autoimmune inflammation affecting multiple joints.
- Post‑traumatic arthritis: Follows fractures or injuries to the hip.
- Avascular necrosis (osteonecrosis): Loss of blood supply to the femoral head leading to collapse and secondary arthritis.
What Causes Knee Arthritis?
- Natural ageing and cartilage wear
- Family history of arthritis
- Previous injuries or fractures
- Carrying extra weight (adds stress to joints)
- Inflammatory conditions (such as rheumatoid arthritis)
- Repetitive movement or high-impact sports
Symptoms & Diagnosis
- Hip or groin pain which often worse with activity and better with rest
- Stiffness in the morning or after sitting
- Reduced range of motion (difficulty putting on shoes, crossing legs)
- Limping or reduced walking distance
- Pain that may refer to the knee or buttock
If symptoms are limiting daily activities or disturbing sleep it’s appropriate to seek specialist advice.
Diagnosis
- Clinical assessment: Detailed history and physical examination looking at range of motion, gait and pain pattern.
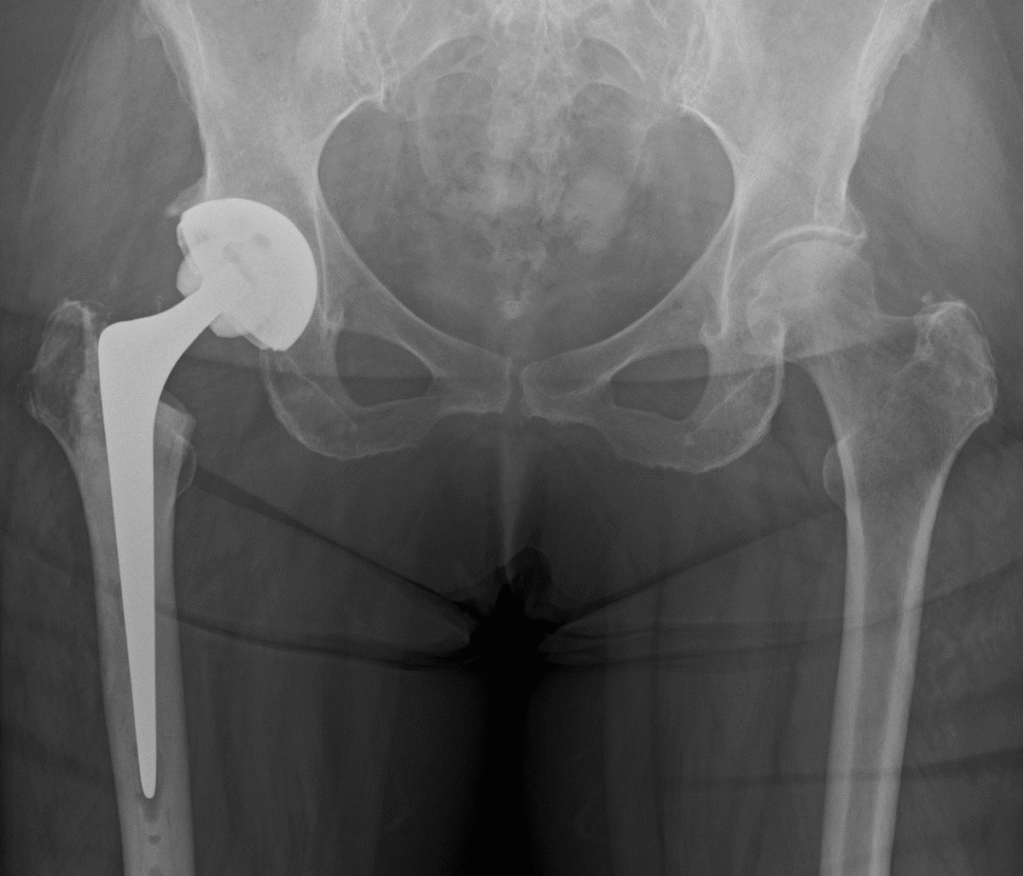
- X‑rays: The primary test to assess joint space, bone spurs and deformity.
- Advanced imaging: MRI or CT scans used selectively (for suspected avascular necrosis, unexplained pain, or pre‑surgical planning).
- Blood tests: To rule out inflammatory causes when suspected.
Treatment Options
Treatment options are tailored to your symptoms, age, activity level and imaging findings. Most people start with conservative measures. Surgery is considered when symptoms significantly affect quality of life despite non‑operative care.
Mr. Radja offers modern techniques including muscle‑sparing approaches and robotic-assisted implantation where appropriate, which may improve precision and early recovery.
What to expect after hip replacement
- Day 0–1: Mobilise with physiotherapy; most patients start walking with aids.
- Weeks 1–6: Pain falls rapidly; continue physiotherapy to rebuild strength and gait.
- 6–12 weeks: Many return to light work and low‑impact activities.
- 3–6 months: Significant functional improvement and most daily activities achievable.
- 12 months: Full recovery and maximal improvement for most patients.
Recovery varies with age, fitness and the exact procedure performed.
Risks & complications
All procedures carry risks. Common and important ones include infection, blood clots, implant wear or loosening, leg‑length difference and dislocation. We will discuss risks specific to your health and planned procedure during consent.
When should you see a specialist?
Please book a consultation if you have:
- Persistent hip or groin pain that limits daily activities
- Worsening stiffness or reduced walking distance
- Symptoms that do not respond to physiotherapy and medications
A specialist appointment includes a focused assessment and a personalised treatment plan.