Table of Contents
What is Patellar Instability (Kneecap Dislocation)?
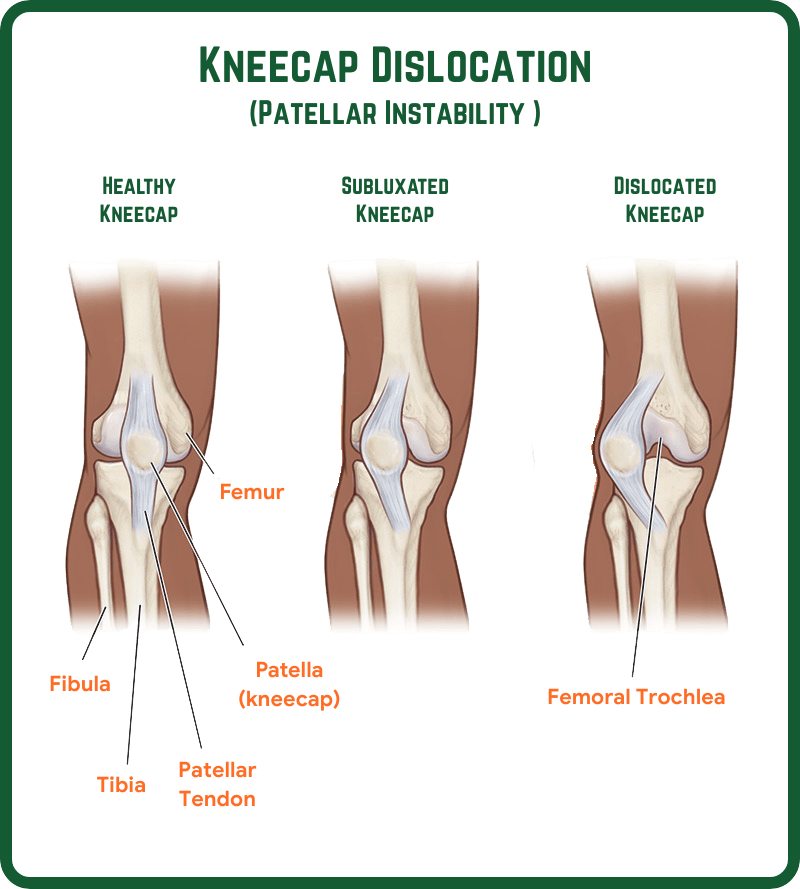
Patellar instability often known as kneecap dislocation occurs when the patella (kneecap) slips out of its normal groove in the thigh bone (femur).
Feel = Sudden Pain + knee is “giving way.”
What Causes Knee to Dislocate?
Patellar instability can result from:
- Trauma or sports injuries – sudden twisting, falls, or impact to the knee.
- Structural factors – such as a high-riding kneecap (patella alta) or a shallow femoral groove (trochlear dysplasia).
- Weak or imbalanced muscles – especially around the thigh and hip, which normally help guide the patella.
- Previous dislocations – once the patella has dislocated, it is more likely to happen again without proper rehabilitation.
Those who are naturally flexible, have alignment issues, or play high-impact sports are at greater risk.
Recognizing the Symptoms
Typical symptoms include:
- Sharp pain around the kneecap
- Swelling and stiffness after the injury
- A feeling that the kneecap has “popped out”
- Difficulty straightening the leg or bearing weight
- Recurrent episodes of the knee “giving way”
If left untreated, repeated dislocations can damage cartilage and increase the risk of early arthritis.
Treatment Options
Treatment depends on whether it’s your first dislocation or a recurring issue.
Summary
Patellar instability is a painful and often recurring condition – but with the right diagnosis, treatment, and rehabilitation, full recovery is achievable. Early assessment by a specialist is key to preventing long-term complications and ensuring optimal knee health.
If you’re struggling with knee instability or repeated dislocations, book a consultation today with Dr. Radja to discuss your best treatment options with a knee specialist in Manchester.
Patella (Kneecap) Instability procedure
Medial patellofemoral ligament (MPFL) reconstruction +/- Tibial Tubercle Osteotomy (TTO)
Patella normally glides smoothly in the groove of the thigh bone (femur), this grove is called trochlea. However, occasionally it may not glide smoothly in the groove (Mal-tracking) leading to patellar instability and worst-case scenario, the patella can dislocate leading to pain and instability
When a patellar dislocation (“coming out of joint”) has occurred the normal ‘restraining’ structures (ligaments) on the inner aspect of the patella may be stretched or torn, making that patient more likely to experience similar episodes when stressing the knee in the future. Conservative management in the form of intensive physiotherapy and taping the patella is often helpful in the first-time patella dislocation, however if the patella dislocates recurrently, then an operation is recommended (MPFL+/-TTO)
What is an MPFL reconstruction?
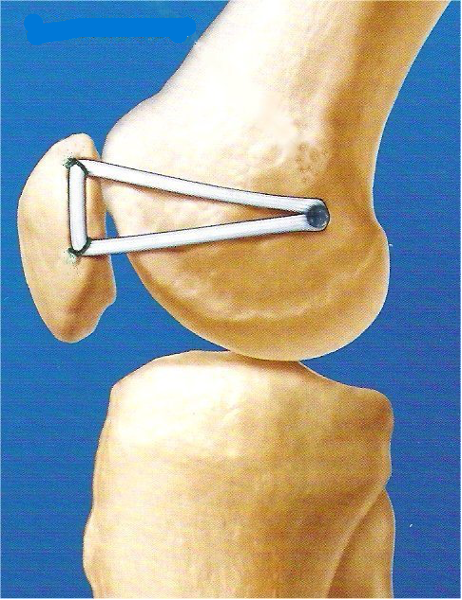
This is the work horse surgery of any kneecap dislocation. MPFL is a ligament that attaches the kneecap to the femoral condyle on the inner side of thigh and is responsible for stabilising the patella to glide on the trochlea especially in the initial stages of knee bending. The function of this ligament can be compared to the reins of a horse – Just like the reins of a horse control the movement of the horse, the MPFL controls the movement of the patella in the trochlea. MPFL reconstruction surgery replaces the native MPFL ligament by a stronger ligament (hamstring tendon) that keeps the patella (kneecap) in place (see image below). The ligament is typically harvested from the hamstrings tendons running on the back of the thigh, by an incision over the inner site of the shin bone (tibia).

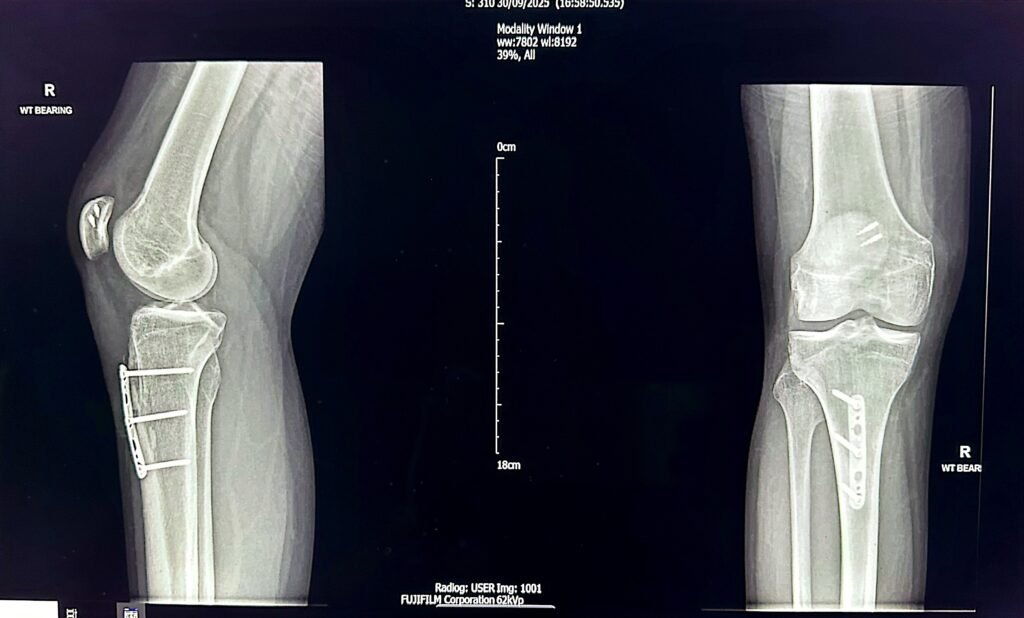
Tibia Tubercle Osteotomy
MPFL reconstruction is often combined with tibial tubercle osteotomy depending on the presenting pathology. This procedure involves the surgical movement of the tibial tuberosity (the area on the shin bone where the patellar tendon attaches) either medially (inwards) or inferiorly or both depending on the risk factors present. The fixation is held with a plate /3-4 screws to hold the repositioned new bone in its new position. It takes 3-4 months for the bones to heal completely.
Below is the X-ray of a young person who has undergone MPFL+TTO surgery 6 months ago, the osteotomy site in tibia has completely healed.
How is the diagnosis made?
Diagnosis is often made by an MRI scan which reveals the integrity of the MPFL ligament. It is also useful to diagnose risk factors including high riding patella (patella alta) and increased TT-TG distance (tibial tuberosity – trochlear groove) & trochlear dysplasia, the three parameters which are often associated with patellar instability.
How is the surgery done?
The procedure is usually performed under general or regional anaesthesia. It typically takes between 60 and 90 minutes and is carried out under a tourniquet. The hamstring tendon is harvested first. The central part of the tendon is then placed into a groove on the inner side of the patella, while the two ends are brought out and inserted into the inner side of the femur at a fixed point identified with the help of X-ray. These ends are then inserted into the drill hole in the femur and secured with an absorbable screw.
Rehabilitation
This procedure is usually done as a day-case, meaning you should be able to go home the same day. Your weight-bearing status will depend on whether a TTO procedure is performed along with the MPFL reconstruction. If only the MPFL surgery is performed, you can fully weight bear immediately after surgery and begin knee bending earlier.
However, if a TTO surgery is also performed, you will be given a brace to control the amount of knee bending during the first 6 weeks to protect the osteotomy site. You will also need to remain non–weight bearing for the first 6 weeks, and your progression to weight bearing will depend on the degree of bone healing.
You will receive physiotherapy to strengthen the muscles and improve the knee’s range of motion.
Return to Normality
You should be able to return to a desk-based job within 6–8 weeks, while normal daily activities can typically be resumed by 3 – 4 months. Driving is usually possible after 6–8 weeks, and flying is generally safe after 3 months. Most patients can return to unrestricted sporting activities around 5 – 6 months post-surgery.
Complications.
As with any surgical procedure, there are potential risks and complications. Specific complications associated with this surgery include:
- Recurrence of dislocation: 3-5%
- Implant failure: 2-3%
- Knee stiffness: 1-3%
- Failure of bone healing: more common in smokers
- Need for revision surgery: occurs in a very small number of patients
